Estrogen & Histamine: The Hidden Hormone Connection
Estrogen & Histamine: The Hidden Hormone Connection
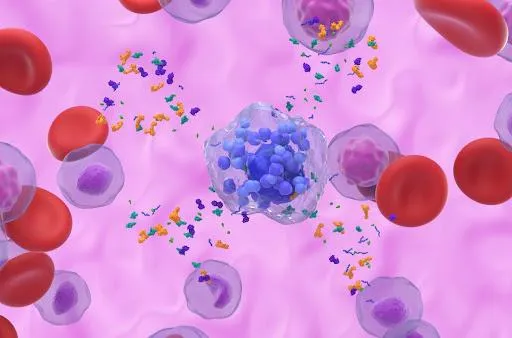
When most people think about hormones, they think of estrogen, progesterone, and testosterone. And when they think of histamine, they think of allergies or antihistamines. But here’s the surprising truth: estrogen and histamine are deeply connected—and this relationship may explain why some people experience migraines, mood changes, allergies, or digestive issues at certain times of the month.
How Estrogen and Histamine Interact
Estrogen triggers histamine release
Estrogen stimulates mast cells—immune cells that store histamine—to release their contents.
More estrogen means more histamine in circulation.
Histamine boosts estrogen
Histamine can also stimulate the ovaries to make more estrogen.
This creates a feedback loop: estrogen increases histamine, and histamine increases estrogen.
Progesterone calms things down
Progesterone helps stabilize mast cells and reduce histamine release.
When progesterone is low—like before a period, during perimenopause, or in cases of “estrogen dominance”—histamine-related symptoms can flare.
Symptoms of the Estrogen–Histamine Connection
When estrogen and histamine rise together, the body can feel the impact in many ways:
Migraines (especially mid-cycle or before periods)
Allergy-like symptoms: runny nose, itchy eyes, hives, flushing
Heavy periods or painful cramps (histamine increases uterine contractions)
Digestive issues: bloating, diarrhea, nausea
Mood shifts: anxiety, irritability, or insomnia (histamine is a wakefulness-promoting neurotransmitter)
This is why symptoms like migraines, allergies, or gut flares often seem worse around ovulation or in the days leading up to a period.

PMDD and Histamine: Can Antihistamines Help?
Premenstrual Dysphoric Disorder (PMDD) is a severe form of PMS marked by mood swings, anxiety, irritability, and sleep disturbances. Since histamine is part of the puzzle, some people have found that taking H1 and H2 blockers (types of antihistamines) during the luteal phase (the two weeks before the period) can ease symptoms.
H1 blockers (like loratadine or cetirizine) target allergy-like symptoms and reduce histamine in tissues.
H2 blockers (like famotidine) reduce histamine’s effects in the gut.
While more research is needed, there is growing anecdotal and clinical support for this approach. For those with PMDD who also notice allergy-like or histamine-driven symptoms, this may be worth discussing with a provider.
What About MCAS?
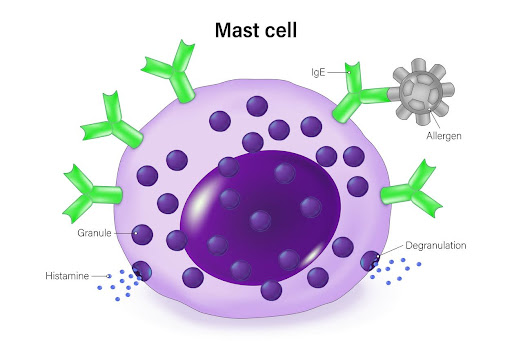
For those with Mast Cell Activation Syndrome (MCAS), this connection is even more important:
Estrogen makes mast cells release more histamine.
Histamine, in turn, stimulates more estrogen production.
This feedback loop can make MCAS flares worse during high-estrogen times of the cycle (ovulation, premenstrual).
Patients with MCAS may notice more hives, flushing, migraines, digestive issues, or anxiety during these windows. Tracking symptoms and hormone cycles can be very helpful, and many benefit from combining mast cell stabilizers (like quercetin, vitamin C, or prescribed meds) with hormone-balancing support.
The Positive Side
The good news? Once you understand the estrogen–histamine connection, you can take steps to predict, track, and manage symptoms. Supporting progesterone, balancing hormones, stabilizing mast cells, and—where appropriate—using targeted antihistamines can make a big difference.
With the right strategy, you can break the estrogen–histamine cycle and feel more in control of your body.
