Autoimmunity and Mold Toxicity: The Hidden Trigger Behind Chronic Illness
Autoimmune diseases are on the rise—and they’re not always easy to explain. For many people, the immune system turns against the body without a clear cause. But what if the answer isn’t just in your genes… but in your environment?
One of the most overlooked triggers for autoimmune disorders is mold toxicity. At Dr. Fox, the Medical Detective, I’ve seen firsthand how hidden mold exposure can quietly drive immune dysfunction, ignite inflammation, and even mimic autoimmune disease.
Let’s uncover the connection.
Mold: The Invisible Invader
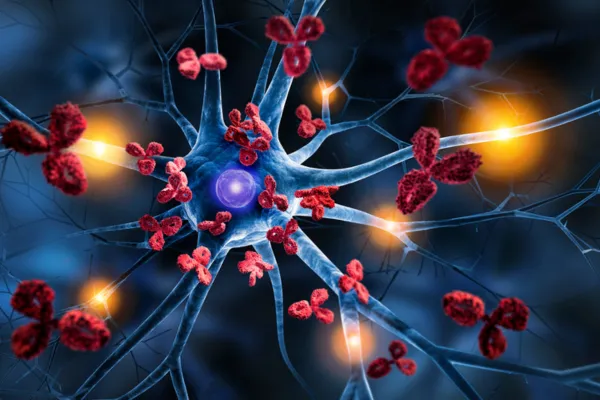
Toxic mold produces mycotoxins, which are small, fat-soluble molecules that can pass through cell membranes, breach the blood-brain barrier, and disrupt immune regulation.
These toxins don’t just cause sinus infections or coughing fits—they can:
Activate proinflammatory cytokines
Disrupt gut barrier integrity (also known as leaky gut)
Trigger immune system confusion
Set off molecular mimicry, where your immune system mistakes your own tissues for invaders
This creates the perfect storm for autoimmune activation.
Research-Backed Links Between Mold and Autoimmunity
Several peer-reviewed studies and clinical observations have linked mold exposure to autoimmune-like conditions:
A 2023 review in Biomolecules highlighted that mycotoxins can impair immune tolerance, increasing risk for autoimmune diseases such as lupus and rheumatoid arthritis [1].
Exposure to Stachybotrys chartarum (black mold) has been shown to activate Th17 immune pathways, a major player in autoimmune inflammation [2].
Mold toxins also disrupt gut microbiota and gut barrier function, key contributors to autoimmunity via the gut-immune axis [3]."
Real-World Patterns I See in Practice
I’ve worked with patients struggling with conditions like:
Hashimoto’s thyroiditis
Lupus
Psoriasis
Multiple sclerosis
Rheumatoid arthritis
In many of these cases, mold exposure was the common denominator—and once identified and addressed, inflammation dropped, flares subsided, and the immune system regained balance.
The issue? Most conventional providers aren’t looking for mold.
How to Tell If Mold Might Be Fueling Your Autoimmune Condition
Ask yourself:
Do your symptoms worsen in specific buildings?
Do you also have fatigue, brain fog, sinus issues, or temperature dysregulation?
Have you had water damage at home or work?
Are conventional treatments helping only a little?
If so, mold could be the missing piece of your medical puzzle.
What You Can Do
Test for mold toxins in your body using urine mycotoxin testing.
Assess your home or workplace with professional mold inspections or dust sampling with an ERMI.
Reduce inflammation with an anti-inflammatory diet and gentle detox support.
Support detox pathways: glutathione, binders, sauna, and lymphatic drainage can help.
Rebuild immune tolerance with gut healing and precision supplementation.
Final Thoughts
Autoimmune conditions don’t just “happen.” Something triggers the immune system to go rogue—and mold is often hiding in plain sight.
If you’ve been living with a diagnosis that doesn’t fully explain your symptoms, or if your autoimmune flares have no clear cause, consider this: the mold might be behind the mystery.
As your Medical Detective, I’m here to help you follow the clues—so you can finally heal.
References
do Nascimento, R. A., et al. (2023). Mycotoxins and autoimmunity: A global perspective. Biomolecules, 13(1), 46. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10251906
Pestka, J. J., et al. (2022). Mycotoxins and the Th17 pathway: Implications for inflammation and autoimmunity. Biomolecules, 13(1), 46. https://doi.org/10.3390/biom13010146
Ouyang, H., et al. (2022). Mold exposure disrupts the gut-immune axis and promotes inflammation. Frontiers in Immunology, 13, 940124. https://doi.org/10.3389/fimmu.2022.940124
